Mood stabilizers should lower the risk of episode recurrence, reduce symptoms overall, and improve our patients' daily function - Journal of Family Practice, March, 2003 by Paul E. Keck, Jr., MD
Bipolar disorder is a persistent, severe, sometimes lethal, and lifelong illness. Therefore, it is important to prevent recurrent mood episodes and suppress intercurrent symptoms. (1) Evidence from randomized, controlled trials supports the efficacy of lithium, carbamazepine (Tegretol), divalproex (Depakote), olanzapine (Zyprexa), and lamotrigine (Lamictal) in long-term treatment of patients with bipolar disorder. As more treatments become available, expectations increase regarding the potential impact of mood stabilizers--in combination with psychotherapeutic interventions--on patients' lives.
Lithium
Alter more than 50 years, lithium remains the cornerstone of bipolar disorder treatment. (2) Lithium is one of the best-studied drugs in acute and long-term treatment, and it remains useful for many patients. On the other hand, new drugs are being developed for maintenance treatment of bipolar disorder because lithium is not effective for everyone and is associated with bothersome side effects for many patients. (2,3)
Goodwin and Jamison found about one-third of patients on lithium monotherapy remained episode-free for about 2 years. (4) Other naturalistic outcome studies of lithium maintenance therapy found somewhat more pessimistic results. A substantial subgroup of patients with bipolar disorder does well on lithium, but we now see greater numbers of patients who do not respond.
These findings imply the question, "What do we expect from mood-stabilizing drugs?" Do we expect complete prevention of mood episodes? These agents are certainly more useful if we define efficacy as a relative reduction in risk of episode recurrence, overall symptom reduction, and improvement in function.
Many factors associated with acute response to lithium--reviewed by Dr. Frye et al in this monograph--are also associated with long-term response. Patients with bipolar I illness--especially with euphoric or elated mania--tend to have better long-term outcomes with lithium than do other patients. Those who have done well on lithium in the past tend continue to do well on lithium, although the number of prior episodes is an important predictor of response.
Carbamazepine
 Numerous studies have examined the use of carbamazepine in bipolar disorder maintenance treatment. (6) In a critical analysis by Dardennes et al of maintenance trials comparing carbamazepine with lithium, three of four studies found the agents comparable in efficacy, and one found lithium more effective than carbamazepine. (7) Limitations inherent in these early maintenance trials led to two recent studies.
Numerous studies have examined the use of carbamazepine in bipolar disorder maintenance treatment. (6) In a critical analysis by Dardennes et al of maintenance trials comparing carbamazepine with lithium, three of four studies found the agents comparable in efficacy, and one found lithium more effective than carbamazepine. (7) Limitations inherent in these early maintenance trials led to two recent studies.
Denicoff et al compared the efficacy of carbamazepine, lithium, and the combination in 52 outpatients with bipolar I disorder. (8) Patients received randomized, double-blind treatment with carbamazepine or lithium in year 1, were crossed over to the alternate agent in year 2, and received the combination in year 3. Adjunctive use of antipsychotics, antidepressants, and benzodiazepines was permitted.
Mean time to a new manic episode was significantly longer with combination therapy (179 days) compared with lithium (90 days) and carbamazepine (66 days) alone. Patients were significantly less likely to experience a manic episode during the combination phase (33%) than with lithium (11%) or carbamazepine (4%). Most patients required adjunctive treatment during each study phase.
Greil et al compared lithium and carbamazepine in an open-label, randomized trial for up to 2.5 years. (9) Some interesting differences between the two medications were noted:
* no significant difference in hospitalization rate, though more carbamazepine-treated patients (55%) than lithium-treated patients (37%) required hospitalization.
* a trend suggesting that carbamazepine was not quite as effective as lithium in preventing recurrence--59% versus 40% (Figure 1).
On the other hand, lithium-treated patients had better outcomes on two measures:
* number of patients who had mood episode recurrence or required an antimanic or antidepressant drug
* mood episode recurrence, need for additional medicine for manic or depressive symptoms, or dropout because of adverse effects.
A post hoc analysis found that patients with bipolar II illness or atypical features--mood incongruence, psychiatric comorbidity, psychotic symptoms and dysphoric mania--tended to do better with carbamazepine than with lithium. (10) These findings are interesting because relatively few predictors of response are found in the literature for carbamazepine maintenance treatment. Taken in total, this study suggested that lithium overall was associated with a better long-term outcome than carbamazepine.
Valproate
Three studies have addressed long-term efficacy of valproate formulations in treating patients with bipolar disorder.
Lambert and Venaud conducted an open comparison trial of valproinide versus lithium in >140 patients. (11) During 18 months, the number of episodes per patient was slightly lower with valpromide (0.5) than with lithium (0.6).
Bowden et al conducted the only placebo-controlled, randomized, maintenance study of valproate in patients with bipolar I disorder (Figure 2). (12) In this 1-year trial, patients received divalproex, lithium, or placebo. The primary outcome measure was time to relapse of any mood episode.
The inclusion of patients with relatively mild bipolar illness probably explains the lack of any significant difference in efficacy among the three treatment groups. Approximately 40% of the patients had never been hospitalized for a manic episode.
Post hoc analysis found divalproex was significantly more effective than placebo in preventing relapse among patients who started divalproex before randomization and then were randomized to divalproex or placebo. This group is representative of clinical practice.
The third maintenance study, which compared divalproex with olanzapine, is described later in this article. (13)
Summary. Predictors of response to valproate are not as well established as for lithium. Predictors of response for maintenance treatment are similar to those identified for acute treatment. Thus far, the evidence suggests that most bipolar illness subtypes--including rapid cycling and mixed mania--have comparable response rates to valproate compared with lithium, leading to the suggestion that valproate may be a broad-spectrum antimanic agent. However, most of these data regarding predictors of response are from open longitudinal studies, not from randomized controlled trials. (14)
Olanzapine
Three randomized, controlled trials have examined olanzapine's efficacy in bipolar disorder maintenance treatment.
Tohen et al compared olanzapine with divalproex over 47 weeks in patients who responded to acute treatment during an initial 3-week trial. (13) Manic symptoms were reduced markedly in the first 3 weeks with both agents, followed by a cumulative reduction in manic symptoms over time following hospital discharge. Throughout the trial, manic symptoms were reduced significantly more in patients receiving olanzapine than divalproex. Depressive symptoms improved similarly in the olanzpaine and divalproex treatment groups.
The second olanzapine maintenance study addressed whether patients who respond to olanzapine plus lithium or valproate should be maintained on the combination. (15) Patients who responded in a 6-week acute treatment trial could either stay on combination treatment or resume monotherapy with lithium or valproate.
A significantly lower relapse rate was found with combination treatment (45%) than with monotherapy (70%). Time to relapse of manic symptoms was significantly longer with combination therapy than with lithium or valproate alone. (15) Combination therapy was significantly more effective in preventing manic relapse but not in preventing depressive relapse (P = 0.07).
Insomnia was significantly more common in the monotherapy group. Weight gain was more common in the combination group (19%) than the monotherapy group (6%).
This is the first large study to compare the efficacy of combination mood-stabilizer treatment with monotherapy over time. A small, 1-year pilot trial comparing lithium plus divalproex versus lithium alone also suggested that combination therapy was more effective. (16)
The third maintenance study of olanzapine was a 1-year comparison with lithium in >400 patients with bipolar I disorder. (17) Patients had clinically significant baseline manic symptoms--YMRS score >20--and at least two manic or mixed episodes within 6 years prior to study entry.
The rate of manic recurrence with olanzapine or lithium did not differ significantly for the first 150 days of the trial, but thereafter the rate was significantly lower for the olanzapine group. Overall, 27% of patients receiving lithium relapsed into mania, compared with 12% of those receiving olanzapine. Fewer patients receiving olanzapine (14%) than lithium (23%) required inpatient admission for relapse. Depression relapse rates did not differ significantly.
Significantly more patients receiving lithium reported insomnia, nausea, and manic symptoms. Significantly more patients receiving olanzapine reported depressive symptoms, somnolence, and weight gain.
Tardive dyskinesia. One other essential question about the safety of olanzapine and any other atypical antipsychotic in bipolar disorder maintenance treatment is whether these agents produce tardive dyskinesia (TD). A 1-year open-label study of olanzapine involving 98 patients with bipolar I disorder found no cases of TD. (18)
Lamotrigine
Two studies--almost identical in design--indicated that lamotrigine was more effective than placebo in delaying time to relapse into bipolar depression. (19,20) The first study randomized patients to lithium, lamotrigine, or placebo after a manic episode was stabilized. (19) The second study used the same randomization scheme but enrolled patients after a bipolar depressive episode was stabilized. (27)
In the first study, lithium and lamotrigine were significantly more effective than placebo in prolonging time to intervention for any mood episode: (20)
* Lamotrigine--but not lithium--was significantly more effective in preventing or extending time to intervention for depression.
*Lithium--but not lamotrigine--was significantly more effective than placebo in delaying time to intervention for a manic episode.
In the second study, lamotrigine and lithium were significantly more effective than placebo in prolonging time to intervention for a mood episode, with no difference between the agents. (27) Only lamotrigine was significantly more effective than placebo in time to intervention for depression. Lithium--but not lamotrigine--was significantly more effective than placebo in time to intervention for mania.
Summary
Data from randomized, controlled trials support the efficacy of lithium, lamotrigine, and olanzapine as foundational agents in long-term treatment of patients with bipolar disorder. Less substantial evidence supports the efficacy of carbamazepine and valproate. Lamotrigine appears to have greater efficacy in preventing bipolar depressive episodes, whereas lithium may have greater efficacy in preventing bipolar manic episodes.
Olanzapine was more effective than lithium in preventing bipolar manic episodes. Olanzapine's efficacy in preventing bipolar depressive episodes requires clarification in placebo-controlled trials. In the few available controlled trials, combination maintenance strategies were more effective in preventing relapse than mood-stabilizer therapies alone.
About the author: Paul E. Keck, Jr., MD is professor of psychiatry, pharmacology and neuroscience, and vice chairman for research in the Department of Psychiatry at the University of Cincinnati College of Medicine. This article appeared in the Journal of Family Practice, March, 2003.
next: Acute Phase of Bipolar Treatment
~ bipolar disorder library
~ all bipolar disorder articles
References
(1.) Judd LL, Akiskal HS, Schettler PJ, et al. The long-term natural history of the weekly symptomatic status of bipolar I disorder. Arch Gen Psychiatry 2002;59:530-7.
(2.) Keck PE, Jr. McElroy SL. Treatment of bipolar disorder. In: Schatzberg AF, Nemeroff CB (eds). The American Psychiatric Textbook of Psychopharmacology (3rd ed). Washington, DC: American Psychiatric Publishing (in press)
(3.) Hirschfeld RM, Bowden CL, Gitlin MJ, et al. Practice guideline for the treatment of patients with bipolar disorder (rev). Am J Psychiatry 2002; 159(suppl):1-50
(4.) Goodwin FK, Jamison KR. Manic-depressive illness. New York: Oxford University Press, 1990.
(5.) Frye MA, Gitlin MJ. Altshuler LL. Treating acute mania. Current Psychiatry 2003; 3(suppl 1):10-13.
(6.) Keck PE, Jr, McElroy SL, Nemeroff CB, Anticonvulsants in the treatment of bipolar disorder. J Neuropsychiatry Clin Neurosci 1992;4:395-405.
(7.) Dardennes R, Even C, Bange F, Heim A. Comparison of carbamazepine and lithium prophylaxis of bipolar disorders. A meta-analysis. Br J Psychiatry 1995;166:378-81.
(8.) Denicoff KD, Smith-Jackson EE, Disney ER, Ali SO. Leverich GS, Post RM. Comparative prophylactic efficacy of lithium, carbamazepine, and the combination in bipolar disorder. J Clin Psychiatry 1997;58:470-8.
(9.) Greil W, Ludwig-Mayerhofer W, Erazo N. et al. Lithium versus carbamazepine in the maintenance treatment of bipolar disorders: a randomised study. J Affect Disord 1997;43:151-61
(10.) Kleindienst N, Greil W. Differential efficacy of lithium and carbamazepine in the prophylaxis of bipolar disorder: results of the MAP study. Neuropsychobiology 2000;42(suppl 1):2-10.
(11.) Lambert P, Venaud G. Comparative study of valpromide versus lithium in the treatment of affective disorders. Nervure 1992;5:57-62
(12.) Bowden CL, Calabrese JR, McElroy SL, et al. A randomized, placebo-controlled 12-month trial of divalproex and lithium in treatment of outpatients with bipolar I disorder. Divalproex Maintenance Study Group. Arch Gen Psychiatry 2000;57:481-9.
(13) Tohen M, Baker RW, Altshuler LL, et al. Olanzapine versus divalproex in the treatment of acute mania. Am J Psychiatry 2002;159:1011-7.
(14.) Calabrese JR, Faremi SH, Kujawa M, Woyshville MJ. Predictors of response to mood stabilizers. J Clin Psychopharmacol 1996;16(suppl 1):S24-31.
(15.) Tohen M, Chengappa KNR, Suppes T, et al. Olanzapine combined with lithium or valproate in the prevention of recurrence in bipolar disorder: an 18-month study (paper presentation). Boston: U.S. Psychiatric and Mental Health Congress annual meeting, 2001.
(16.) Solomon DA, Ryan CE, Keitner GI, et al. A pilot study of lithium carbonate plus divalproex sodium for the continuation and maintenance treatment of patients with bipolar I disorder. J Clin Psychiatry 1997;58:95-9.
(17.) Tohen M. Marneros A, Bowden CL, et al. Olanzapine versus lithium in relapse prevention in bipolar disorder: a randomized double-blind controlled 12-month clinical trial (paper presentation). Freiburg, Germany: European Stanley Foundation Bipolar Conference, 2002.
(18.) Sunger TM, Grundy SL, Gibson PJ, Namjoshi MA, Greaney MG, Tohen ME Long-term olanzapine therapy in the treatment of bipolar I disorder: an open-label continuation phase study. J Clin Psychiatry 2001;62:273-81.
(19.) Calabrese JR, Shelton MD, Rapport DJ. Kimmel SE, Eljah O, Long-term treatment of bipolar disorder with lamotrigine J Clin Psychiatry 2002;63(suppl 10):18-22.
(20.) Bowden CL. Lamotrigine in the treatment of bipolar disorder. Expert Opin Pharmacother 2002;3:1513-9
next: Acute Phase of Bipolar Treatment
~ bipolar disorder library
~ all bipolar disorder articles
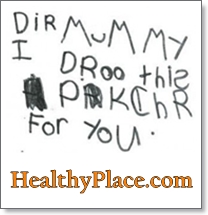 Dyslexia is an inherited condition that makes it extremely difficult to read, write, and spell in your native language -- despite at least average intelligence. Dyslexia is a neurologically-based disorder which interferes with the acquisition and processing of language. Varying in degrees of severity, it is manifested by difficulties in receptive and expressive language, including phonological processing, in reading, writing, spelling, handwriting, and sometimes in arithmetic.
Dyslexia is an inherited condition that makes it extremely difficult to read, write, and spell in your native language -- despite at least average intelligence. Dyslexia is a neurologically-based disorder which interferes with the acquisition and processing of language. Varying in degrees of severity, it is manifested by difficulties in receptive and expressive language, including phonological processing, in reading, writing, spelling, handwriting, and sometimes in arithmetic. I'd like to set aside some space and time to focus on advocating. I believe that learning to advocate is a must for any parent, especially those of us who have been blessed with special children. One of the most important skills one can have is proper communication. It's one thing to know what needs to be done and what services you need and its another thing to get your wants and wishes across. The last thing you want to do is alienate the very people you need to make your ADHD child's school experience a successful and positive one.
I'd like to set aside some space and time to focus on advocating. I believe that learning to advocate is a must for any parent, especially those of us who have been blessed with special children. One of the most important skills one can have is proper communication. It's one thing to know what needs to be done and what services you need and its another thing to get your wants and wishes across. The last thing you want to do is alienate the very people you need to make your ADHD child's school experience a successful and positive one.
 There is a mismatch between patients' own descriptions of anxiety after a heart attack and the way it is recorded and treated by their doctors. Anxiety is common - but not inevitable - after a heart attack. Left untreated, it may impair a patient's recovery.
There is a mismatch between patients' own descriptions of anxiety after a heart attack and the way it is recorded and treated by their doctors. Anxiety is common - but not inevitable - after a heart attack. Left untreated, it may impair a patient's recovery. In the manic phase, they usually feel invincible, euphoric, hyperactive, and very productive. This could lead to excessively risky behavior, grand delusions, uncontrollable thoughts and actions, irritability, rage, and insomnia. In the depressed phase, they can experience intense sadness, despair, fatigue, insomnia, difficulty concentrating, changes in appetite, and constant thoughts of suicide.
In the manic phase, they usually feel invincible, euphoric, hyperactive, and very productive. This could lead to excessively risky behavior, grand delusions, uncontrollable thoughts and actions, irritability, rage, and insomnia. In the depressed phase, they can experience intense sadness, despair, fatigue, insomnia, difficulty concentrating, changes in appetite, and constant thoughts of suicide. Numerous studies have examined the use of
Numerous studies have examined the use of  Increasingly, mood disorders are becoming well-defined and recognized among patients and healthcare providers. However, these conditions are relegated to being connected to ovarian activity (i.e., premenstrual, post-partum or menopausal) and thus hormonally dominated. Missing from the wealth of understanding is the fact that anxiety symptoms are an important and overlooked component of each of these disorders, according to data presented today at the Anxiety Disorders Association of America's 23rd annual meeting here.
Increasingly, mood disorders are becoming well-defined and recognized among patients and healthcare providers. However, these conditions are relegated to being connected to ovarian activity (i.e., premenstrual, post-partum or menopausal) and thus hormonally dominated. Missing from the wealth of understanding is the fact that anxiety symptoms are an important and overlooked component of each of these disorders, according to data presented today at the Anxiety Disorders Association of America's 23rd annual meeting here. After two hours of public comment and committee debate, the House Health and Human Services Committee voted to adjourn without voting. That means the committee could continue discussion of the bill later in the session.
After two hours of public comment and committee debate, the House Health and Human Services Committee voted to adjourn without voting. That means the committee could continue discussion of the bill later in the session.