Deciding when to share your diagnosis of posttraumatic stress disorder (PTSD), and with whom, can be difficult to do. Even though talking about PTSD and seeking support from others is an important step toward recovery, choosing who and when to share your diagnosis of PTSD may be stressful and anxiety producing. The uncertainty of how others will react to hearing that you have a mental health issue can be as troubling as dealing with mental illness itself (Stigma Busting: Things Not to Say to Anxious People). There are some ways though, to decide who and when to tell about your PTSD diagnosis.
Trauma! A PTSD Blog
For recovery from posttraumatic stress disorder (PTSD), it is important to have a safe place. One time a friend asked, “Dan, have you ever felt safe anywhere?” For years I walked around constantly on high alert and my posttraumatic stress disorder was on full display. Since I grew up in a household where violent domestic abuse occurred, it has been important for me to establish my own safe place in PTSD recovery where I can relax (How to Develop a Safe Place For Mental Illness Recovery).
Using mindfulness in posttraumatic stress disorder (PTSD) recovery can be a lifesaver. One of the most difficult things about having PTSD is dealing with the PTSD symptoms -- but mindfulness can help, even when triggered. There are a number of things that I know will trigger me, and I do my best to avoid those triggers. Some things sneak up on me, though, and I have to deal with the anxiety and fear that is caused by the fight or flight response my body has. One of the most effective ways I have found to get through those types of situations is by using mindfulness in my PTSD recovery.
There are many things that can trigger my posttraumatic stress disorder (PTSD). Over the years, I have learned to adapt pretty well to living with posttraumatic stress disorder. But certain situations or settings can trigger, which means to cause an onset of, the anxiety of my PTSD, taking me back to a time when I wasn’t safe and my life was in danger. I will become hypervigilant, begin to dissociate, and feel extreme anxiety. I’ve learned to watch for those situations, and to find effective coping mechanisms that reduce my anxiety when my PTSD gets triggered.
A posttraumatic stress disorder (PTSD) recovery program often requires a network of supporters for the PTSD sufferer that includes loved ones, friends, doctors and even coworkers. This is because posttraumatic stress disorder doesn't only affect those who are diagnosed with it. Usually, many people play a part in the sufferer's PTSD recovery program. Sometimes it's hard to know how to handle it when someone with PTSD is triggered, anxious, or depressed -- what to say or do to make the situations better. These are muddy waters to navigate, but it can be done. You are able to help someone through their PTSD recovery program.
One of the biggest myths about posttraumatic stress disorder (PTSD) is that those who have PTSD have a mental weakness. I understand why people think that way. When I was plagued with flashbacks, nightmares and disruptive thoughts about my past trauma, I believed that was a sign of my mental weakness. But it is a myth that people with PTSD have mental weakness. As a matter of fact, we are some of the strongest people I know.
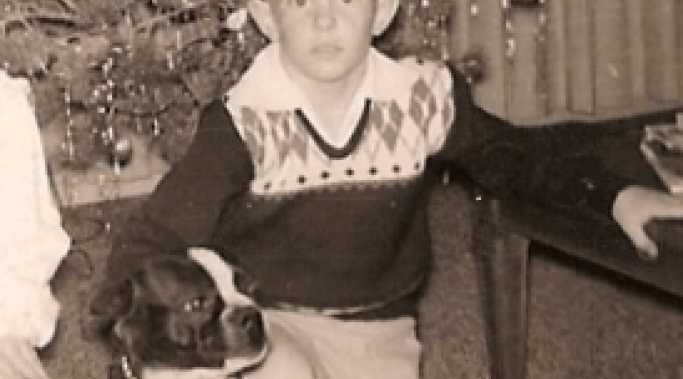
I have received enormous benefit to my PTSD recovery from the use of inner child exercises. Inner child exercises help heal the wounded child who lived for so many years within my body. It was that damaged child who suffered the abuse that led to my posttraumatic stress disorder (PTSD).
When I was first presented the concept of inner child work, I thought it sounded silly. But in a time of great desperation, I tried it, with the most remarkable results. My PTSD recovery is greatly benefitted by using inner child exercises. Here's how they work.
Dealing with body memories in posttraumatic stress disorder (PTSD) recovery is one of the most difficult symptoms. Body memories differ from flashbacks. A flashback is a sudden, vivid memory that makes you feel like you are experiencing your trauma all over again. It's a physical feeling of being there, not just a normal memory where you are recalling what has happened. However, body memories are another type of way we relive trauma that, while far less intense, are still upsetting. Body memories are not so easily identified; they can cause mental problems for years before you recognize them as a body memory.
Developing a sense of personal safety and establishing boundaries is a very important when dealing with my symptoms of posttraumatic stress disorder (PTSD). I can tremendously reduce my anxiety and hypervigilance through creating a safe space for myself. I do this by establishing boundaries as part of my PTSD recovery.
Before being diagnosed with posttraumatic stress disorder (PTSD), I thought that my biggest issue was alcoholism. What I didn't understand was that there was a direct link between my drinking and dealing with my PTSD symptoms. I was self-medicating to control my symptoms without even knowing it.