Onglyza for Treatment of Diabetes - Full Prescribing Information
Brand Name: Onglyza
Generic Name: Saxagliptin
Dosage Form: tablet, film coated
Contents:
Indications and Usage
Dosage and Administration
Dosage Forms and Strengths
Contraindications
Warnings and Precautions
Adverse Reactions
Drug Interactions
Use in Specific Populations
Overdosage
Description
Pharmacology
Nonclinical Toxicology
Clinical Studies
How Supplied
Onglyza patient information (in plain English)
Indications and Usage
Monotherapy and Combination Therapy
Onglyza is indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus. [See Clinical Studies].
Important Limitations of Use
Onglyza should not be used for the treatment of type 1 diabetes mellitus or diabetic ketoacidosis, as it would not be effective in these settings.
Onglyza has not been studied in combination with insulin.
Dosage and Administration
Recommended Dosing
The recommended dose of Onglyza is 2.5 mg or 5 mg once daily taken regardless of meals.
Patients with Renal Impairment
No dosage adjustment for Onglyza is recommended for patients with mild renal impairment (creatinine clearance [CrCl] >50 mL/min).
The dose of Onglyza is 2.5 mg once daily for patients with moderate or severe renal impairment, or with end-stage renal disease (ESRD) requiring hemodialysis (creatinine clearance [CrCl] ≤50 mL/min). Onglyza should be administered following hemodialysis. Onglyza has not been studied in patients undergoing peritoneal dialysis.
Because the dose of Onglyza should be limited to 2.5 mg based upon renal function, assessment of renal function is recommended prior to initiation of Onglyza and periodically thereafter. Renal function can be estimated from serum creatinine using the Cockcroft-Gault formula or Modification of Diet in Renal Disease formula. [See Clinical Pharmacology, Pharmacokinetics.]
Strong CYP3A4/5 Inhibitors
The dose of Onglyza is 2.5 mg once daily when coadministered with strong cytochrome P450 3A4/5 (CYP3A4/5) inhibitors (e.g., ketoconazole, atazanavir, clarithromycin, indinavir, itraconazole, nefazodone, nelfinavir, ritonavir, saquinavir, and telithromycin). [See Drug Interactions, Inhibitors of CYP3A4/5 Enzymes and Clinical Pharmacology, Pharmacokinetics.]
Dosage Forms and Strengths
- Onglyza (saxagliptin) 5 mg tablets are pink, biconvex, round, film-coated tablets with "5" printed on one side and "4215" printed on the reverse side, in blue ink.
- Onglyza (saxagliptin) 2.5 mg tablets are pale yellow to light yellow, biconvex, round, film-coated tablets with "2.5" printed on one side and "4214" printed on the reverse side, in blue ink.
Contraindications
None.
Warnings and Precautions
Use with Medications Known to Cause Hypoglycemia
Insulin secretagogues, such as sulfonylureas, cause hypoglycemia. Therefore, a lower dose of the insulin secretagogue may be required to reduce the risk of hypoglycemia when used in combination with Onglyza. [See Adverse Reactions, Clinical Trials Experience.]
Macrovascular Outcomes
There have been no clinical studies establishing conclusive evidence of macrovascular risk reduction with Onglyza or any other antidiabetic drug.
Adverse Reactions
Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Monotherapy and Add-On Combination Therapy
In two placebo-controlled monotherapy trials of 24-weeks duration, patients were treated with Onglyza 2.5 mg daily, Onglyza 5 mg daily, and placebo. Three 24-week, placebo-controlled, add-on combination therapy trials were also conducted: one with metformin, one with a thiazolidinedione (pioglitazone or rosiglitazone), and one with glyburide. In these three trials, patients were randomized to add-on therapy with Onglyza 2.5 mg daily, Onglyza 5 mg daily, or placebo. A saxagliptin 10 mg treatment arm was included in one of the monotherapy trials and in the add-on combination trial with metformin.
In a prespecified pooled analysis of the 24-week data (regardless of glycemic rescue) from the two monotherapy trials, the add-on to metformin trial, the add-on to thiazolidinedione (TZD) trial, and the add-on to glyburide trial, the overall incidence of adverse events in patients treated with Onglyza 2.5 mg and Onglyza 5 mg was similar to placebo (72.0% and 72.2% versus 70.6%, respectively). Discontinuation of therapy due to adverse events occurred in 2.2%, 3.3%, and 1.8% of patients receiving Onglyza 2.5 mg, Onglyza 5 mg, and placebo, respectively. The most common adverse events (reported in at least 2 patients treated with Onglyza 2.5 mg or at least 2 patients treated with Onglyza 5 mg) associated with premature discontinuation of therapy included lymphopenia (0.1% and 0.5% versus 0%, respectively), rash (0.2% and 0.3% versus 0.3%), blood creatinine increased (0.3% and 0% versus 0%), and blood creatine phosphokinase increased (0.1% and 0.2% versus 0%). The adverse reactions in this pooled analysis reported (regardless of investigator assessment of causality) in ≥5% of patients treated with Onglyza 5 mg, and more commonly than in patients treated with placebo are shown in Table 1.
Table 1: Adverse Reactions (Regardless of Investigator Assessment of Causality) in Placebo-Controlled Trials* Reported in ≥5% of Patients Treated with Onglyza 5 mg and More Commonly than in Patients Treated with Placebo
| Number (%) of Patients | ||
|---|---|---|
| Onglyza 5 mg N=882 | Placebo N=799 | |
| * The 5 placebo-controlled trials include two monotherapy trials and one add-on combination therapy trial with each of the following: metformin, thiazolidinedione, or glyburide. Table shows 24-week data regardless of glycemic rescue. | ||
| Upper respiratory tract infection | 68 (7.7) | 61 (7.6) |
| Urinary tract infection | 60 (6.8) | 49 (6.1) |
| Headache | 57 (6.5) | 47 (5.9) |
In patients treated with Onglyza 2.5 mg, headache (6.5%) was the only adverse reaction reported at a rate ≥5% and more commonly than in patients treated with placebo.
In this pooled analysis, adverse reactions that were reported in ≥2% of patients treated with Onglyza 2.5 mg or Onglyza 5 mg and ≥1% more frequently compared to placebo included: sinusitis (2.9% and 2.6% versus 1.6%, respectively), abdominal pain (2.4% and 1.7% versus 0.5%), gastroenteritis (1.9% and 2.3% versus 0.9%), and vomiting (2.2% and 2.3% versus 1.3%).
In the add-on to TZD trial, the incidence of peripheral edema was higher for Onglyza 5 mg versus placebo (8.1% and 4.3%, respectively). The incidence of peripheral edema for Onglyza 2.5 mg was 3.1%. None of the reported adverse reactions of peripheral edema resulted in study drug discontinuation. Rates of peripheral edema for Onglyza 2.5 mg and Onglyza 5 mg versus placebo were 3.6% and 2% versus 3% given as monotherapy, 2.1% and 2.1% versus 2.2% given as add-on therapy to metformin, and 2.4% and 1.2% versus 2.2% given as add-on therapy to glyburide.
The incidence rate of fractures was 1.0 and 0.6 per 100 patient-years, respectively, for Onglyza (pooled analysis of 2.5 mg, 5 mg, and 10 mg) and placebo. The incidence rate of fracture events in patients who received Onglyza did not increase over time. Causality has not been established and nonclinical studies have not demonstrated adverse effects of saxagliptin on bone.
An event of thrombocytopenia, consistent with a diagnosis of idiopathic thrombocytopenic purpura, was observed in the clinical program. The relationship of this event to Onglyza is not known.
Adverse Reactions Associated with Onglyza Coadministered with Metformin in Treatment-Naive Patients with Type 2 Diabetes
Table 2 shows the adverse reactions reported (regardless of investigator assessment of causality) in ≥5% of patients participating in an additional 24-week, active-controlled trial of coadministered Onglyza and metformin in treatment-naive patients.
Table 2: Initial Therapy with Combination of Onglyza and Metformin in Treatment-Naive Patients: Adverse Reactions Reported (Regardless of Investigator Assessment of Causality) in ≥5% of Patients Treated with Combination Therapy of Onglyza 5 mg Plus Metformin (and More Commonly than in Patients Treated with Metformin Alone)
| Number (%) of Patients | ||
|---|---|---|
| Onglyza 5 mg + Metformin* N=320 | Metformin* N=328 | |
| * Metformin was initiated at a starting dose of 500 mg daily and titrated up to a maximum of 2000 mg daily. | ||
| Headache | 24 (7.5) | 17 (5.2) |
| Nasopharyngitis | 22 (6.9) | 13 (4.0) |
Hypoglycemia
Adverse reactions of hypoglycemia were based on all reports of hypoglycemia; a concurrent glucose measurement was not required. In the add-on to glyburide study, the overall incidence of reported hypoglycemia was higher for Onglyza 2.5 mg and Onglyza 5 mg (13.3% and 14.6%) versus placebo (10.1%). The incidence of confirmed hypoglycemia in this study, defined as symptoms of hypoglycemia accompanied by a fingerstick glucose value of ≤50 mg/dL, was 2.4% and 0.8% for Onglyza 2.5 mg and Onglyza 5 mg and 0.7% for placebo. The incidence of reported hypoglycemia for Onglyza 2.5 mg and Onglyza 5 mg versus placebo given as monotherapy was 4.0% and 5.6% versus 4.1%, respectively, 7.8% and 5.8% versus 5% given as add-on therapy to metformin, and 4.1% and 2.7% versus 3.8% given as add-on therapy to TZD. The incidence of reported hypoglycemia was 3.4% in treatment-naive patients given Onglyza 5 mg plus metformin and 4.0% in patients given metformin alone.
Hypersensitivity Reactions
Hypersensitivity-related events, such as urticaria and facial edema in the 5-study pooled analysis up to Week 24 were reported in 1.5%, 1.5%, and 0.4% of patients who received Onglyza 2.5 mg, Onglyza 5 mg, and placebo, respectively. None of these events in patients who received Onglyza required hospitalization or were reported as life-threatening by the investigators. One saxagliptin-treated patient in this pooled analysis discontinued due to generalized urticaria and facial edema.
Vital Signs
No clinically meaningful changes in vital signs have been observed in patients treated with Onglyza.
Laboratory Tests
Absolute Lymphocyte Counts
There was a dose-related mean decrease in absolute lymphocyte count observed with Onglyza. From a baseline mean absolute lymphocyte count of approximately 2200 cells/microL, mean decreases of approximately 100 and 120 cells/microL with Onglyza 5 mg and 10 mg, respectively, relative to placebo were observed at 24 weeks in a pooled analysis of five placebo-controlled clinical studies. Similar effects were observed when Onglyza 5 mg was given in initial combination with metformin compared to metformin alone. There was no difference observed for Onglyza 2.5 mg relative to placebo. The proportion of patients who were reported to have a lymphocyte count ≤750 cells/microL was 0.5%, 1.5%, 1.4%, and 0.4% in the saxagliptin 2.5 mg, 5 mg, 10 mg, and placebo groups, respectively. In most patients, recurrence was not observed with repeated exposure to Onglyza although some patients had recurrent decreases upon rechallenge that led to discontinuation of Onglyza. The decreases in lymphocyte count were not associated with clinically relevant adverse reactions.
The clinical significance of this decrease in lymphocyte count relative to placebo is not known. When clinically indicated, such as in settings of unusual or prolonged infection, lymphocyte count should be measured. The effect of Onglyza on lymphocyte counts in patients with lymphocyte abnormalities (e.g., human immunodeficiency virus) is unknown.
Platelets
Onglyza did not demonstrate a clinically meaningful or consistent effect on platelet count in the six, double-blind, controlled clinical safety and efficacy trials.
Drug Interactions
Inducers of CYP3A4/5 Enzymes
Rifampin significantly decreased saxagliptin exposure with no change in the area under the time-concentration curve (AUC) of its active metabolite, 5-hydroxy saxagliptin. The plasma dipeptidyl peptidase-4 (DPP4) activity inhibition over a 24-hour dose interval was not affected by rifampin. Therefore, dosage adjustment of Onglyza is not recommended. [See Clinical Pharmacology, Pharmacokinetics.]
Inhibitors of CYP3A4/5 Enzymes
Moderate Inhibitors of CYP3A4/5
Diltiazem increased the exposure of saxagliptin. Similar increases in plasma concentrations of saxagliptin are anticipated in the presence of other moderate CYP3A4/5 inhibitors (e.g., amprenavir, aprepitant, erythromycin, fluconazole, fosamprenavir, grapefruit juice, and verapamil); however, dosage adjustment of Onglyza is not recommended. [See Clinical Pharmacology, Pharmacokinetics.]
Strong Inhibitors of CYP3A4/5
Ketoconazole significantly increased saxagliptin exposure. Similar significant increases in plasma concentrations of saxagliptin are anticipated with other strong CYP3A4/5 inhibitors (e.g., atazanavir, clarithromycin, indinavir, itraconazole, nefazodone, nelfinavir, ritonavir, saquinavir, and telithromycin). The dose of Onglyza should be limited to 2.5 mg when coadministered with a strong CYP3A4/5 inhibitor. [See Dosage and Administration, Strong CYP3A4/5 Inhibitors and Clinical Pharmacology, Pharmacokinetics.]
Use in Specific Populations
Pregnancy
Pregnancy Category B
There are no adequate and well-controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, Onglyza, like other antidiabetic medications, should be used during pregnancy only if clearly needed.
Saxagliptin was not teratogenic at any dose tested when administered to pregnant rats and rabbits during periods of organogenesis. Incomplete ossification of the pelvis, a form of developmental delay, occurred in rats at a dose of 240 mg/kg, or approximately 1503 and 66 times human exposure to saxagliptin and the active metabolite, respectively, at the maximum recommended human dose (MRHD) of 5 mg. Maternal toxicity and reduced fetal body weights were observed at 7986 and 328 times the human exposure at the MRHD for saxagliptin and the active metabolite, respectively. Minor skeletal variations in rabbits occurred at a maternally toxic dose of 200 mg/kg, or approximately 1432 and 992 times the MRHD. When administered to rats in combination with metformin, saxagliptin was not teratogenic nor embryolethal at exposures 21 times the saxagliptin MRHD. Combination administration of metformin with a higher dose of saxagliptin (109 times the saxagliptin MRHD) was associated with craniorachischisis (a rare neural tube defect characterized by incomplete closure of the skull and spinal column) in two fetuses from a single dam. Metformin exposures in each combination were 4 times the human exposure of 2000 mg daily.
Saxagliptin administered to female rats from gestation day 6 to lactation day 20 resulted in decreased body weights in male and female offspring only at maternally toxic doses (exposures ≥1629 and 53 times saxagliptin and its active metabolite at the MRHD). No functional or behavioral toxicity was observed in offspring of rats administered saxagliptin at any dose.
Saxagliptin crosses the placenta into the fetus following dosing in pregnant rats.
Nursing Mothers
Saxagliptin is secreted in the milk of lactating rats at approximately a 1:1 ratio with plasma drug concentrations. It is not known whether saxagliptin is secreted in human milk. Because many drugs are secreted in human milk, caution should be exercised when Onglyza is administered to a nursing woman.
Pediatric Use
Safety and effectiveness of Onglyza in pediatric patients have not been established.
Geriatric Use
In the six, double-blind, controlled clinical safety and efficacy trials of Onglyza, 634 (15.3%) of the 4148 randomized patients were 65 years and over, and 59 (1.4%) patients were 75 years and over. No overall differences in safety or effectiveness were observed between patients ≥65 years old and the younger patients. While this clinical experience has not identified differences in responses between the elderly and younger patients, greater sensitivity of some older individuals cannot be ruled out.
Saxagliptin and its active metabolite are eliminated in part by the kidney. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection in the elderly based on renal function. [See Dosage and Administration, Patients with Renal Impairment and Clinical Pharmacology, Pharmacokinetics.]
Overdosage
In a controlled clinical trial, once-daily, orally-administered Onglyza in healthy subjects at doses up to 400 mg daily for 2 weeks (80 times the MRHD) had no dose-related clinical adverse reactions and no clinically meaningful effect on QTc interval or heart rate.
In the event of an overdose, appropriate supportive treatment should be initiated as dictated by the patient's clinical status. Saxagliptin and its active metabolite are removed by hemodialysis (23% of dose over 4 hours).
Description
Saxagliptin is an orally-active inhibitor of the DPP4 enzyme.
Saxagliptin monohydrate is described chemically as (1S,3S,5S)-2-[(2S)-2-Amino-2-(3-hydroxytricyclo[3.3.1.13,7]dec-1-yl)acetyl]-2-azabicyclo[3.1.0]hexane-3-carbonitrile, monohydrate or (1S,3S,5S) - 2 - [(2S) - 2 - Amino - 2 - (3 - hydroxyadamantan - 1 - yl)acetyl] - 2 - azabicyclo[3.1.0]hexane - 3 - carbonitrile hydrate. The empirical formula is C18H25N3O2-H2O and the molecular weight is 333.43. The structural formula is:
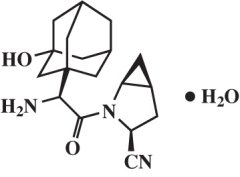
Saxagliptin monohydrate is a white to light yellow or light brown, non-hygroscopic, crystalline powder. It is sparingly soluble in water at 24°C ± 3°C, slightly soluble in ethyl acetate, and soluble in methanol, ethanol, isopropyl alcohol, acetonitrile, acetone, and polyethylene glycol 400 (PEG 400).
Each film-coated tablet of Onglyza for oral use contains either 2.79 mg saxagliptin hydrochloride (anhydrous) equivalent to 2.5 mg saxagliptin or 5.58 mg saxagliptin hydrochloride (anhydrous) equivalent to 5 mg saxagliptin and the following inactive ingredients: lactose monohydrate, microcrystalline cellulose, croscarmellose sodium, and magnesium stearate. In addition, the film coating contains the following inactive ingredients: polyvinyl alcohol, polyethylene glycol, titanium dioxide, talc, and iron oxides.
Clinical Pharmacology
Mechanism of Action
Increased concentrations of the incretin hormones such as glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic polypeptide (GIP) are released into the bloodstream from the small intestine in response to meals. These hormones cause insulin release from the pancreatic beta cells in a glucose-dependent manner but are inactivated by the dipeptidyl peptidase-4 (DPP4) enzyme within minutes. GLP-1 also lowers glucagon secretion from pancreatic alpha cells, reducing hepatic glucose production. In patients with type 2 diabetes, concentrations of GLP-1 are reduced but the insulin response to GLP-1 is preserved. Saxagliptin is a competitive DPP4 inhibitor that slows the inactivation of the incretin hormones, thereby increasing their bloodstream concentrations and reducing fasting and postprandial glucose concentrations in a glucose-dependent manner in patients with type 2 diabetes mellitus.
Pharmacodynamics
In patients with type 2 diabetes mellitus, administration of Onglyza inhibits DPP4 enzyme activity for a 24-hour period. After an oral glucose load or a meal, this DPP4 inhibition resulted in a 2- to 3-fold increase in circulating levels of active GLP-1 and GIP, decreased glucagon concentrations, and increased glucose-dependent insulin secretion from pancreatic beta cells. The rise in insulin and decrease in glucagon were associated with lower fasting glucose concentrations and reduced glucose excursion following an oral glucose load or a meal.
Cardiac Electrophysiology
In a randomized, double-blind, placebo-controlled, 4-way crossover, active comparator study using moxifloxacin in 40 healthy subjects, Onglyza was not associated with clinically meaningful prolongation of the QTc interval or heart rate at daily doses up to 40 mg (8 times the MRHD).
Pharmacokinetics
The pharmacokinetics of saxagliptin and its active metabolite, 5-hydroxy saxagliptin were similar in healthy subjects and in patients with type 2 diabetes mellitus. The Cmax and AUC values of saxagliptin and its active metabolite increased proportionally in the 2.5 to 400 mg dose range. Following a 5 mg single oral dose of saxagliptin to healthy subjects, the mean plasma AUC values for saxagliptin and its active metabolite were 78 ng-h/mL and 214 ng-h/mL, respectively. The corresponding plasma Cmax values were 24 ng/mL and 47 ng/mL, respectively. The average variability (%CV) for AUC and Cmax for both saxagliptin and its active metabolite was less than 25%.
No appreciable accumulation of either saxagliptin or its active metabolite was observed with repeated once-daily dosing at any dose level. No dose- and time-dependence were observed in the clearance of saxagliptin and its active metabolite over 14 days of once-daily dosing with saxagliptin at doses ranging from 2.5 to 400 mg.
Absorption
The median time to maximum concentration (Tmax) following the 5 mg once daily dose was 2 hours for saxagliptin and 4 hours for its active metabolite. Administration with a high-fat meal resulted in an increase in Tmax of saxagliptin by approximately 20 minutes as compared to fasted conditions. There was a 27% increase in the AUC of saxagliptin when given with a meal as compared to fasted conditions. Onglyza may be administered with or without food.
Distribution
The in vitro protein binding of saxagliptin and its active metabolite in human serum is negligible. Therefore, changes in blood protein levels in various disease states (e.g., renal or hepatic impairment) are not expected to alter the disposition of saxagliptin.
Metabolism
The metabolism of saxagliptin is primarily mediated by cytochrome P450 3A4/5 (CYP3A4/5). The major metabolite of saxagliptin is also a DPP4 inhibitor, which is one-half as potent as saxagliptin. Therefore, strong CYP3A4/5 inhibitors and inducers will alter the pharmacokinetics of saxagliptin and its active metabolite. [See Drug Interactions.]
Excretion
Saxagliptin is eliminated by both renal and hepatic pathways. Following a single 50 mg dose of 14C-saxagliptin, 24%, 36%, and 75% of the dose was excreted in the urine as saxagliptin, its active metabolite, and total radioactivity, respectively. The average renal clearance of saxagliptin (~230 mL/min) was greater than the average estimated glomerular filtration rate (~120 mL/min), suggesting some active renal excretion. A total of 22% of the administered radioactivity was recovered in feces representing the fraction of the saxagliptin dose excreted in bile and/or unabsorbed drug from the gastrointestinal tract. Following a single oral dose of Onglyza 5 mg to healthy subjects, the mean plasma terminal half-life (t1/2) for saxagliptin and its active metabolite was 2.5 and 3.1 hours, respectively.
Specific Populations
Renal Impairment
A single-dose, open-label study was conducted to evaluate the pharmacokinetics of saxagliptin (10 mg dose) in subjects with varying degrees of chronic renal impairment (N=8 per group) compared to subjects with normal renal function. The study included patients with renal impairment classified on the basis of creatinine clearance as mild (>50 to ≤80 mL/min), moderate (30 to ≤50 mL/min), and severe (<30 mL/min), as well as patients with end-stage renal disease on hemodialysis. Creatinine clearance was estimated from serum creatinine based on the Cockcroft-Gault formula:
CrCl = [140 − age (years)] × weight (kg) {× 0.85 for female patients}
[72 × serum creatinine (mg/dL)]
The degree of renal impairment did not affect the Cmax of saxagliptin or its active metabolite. In subjects with mild renal impairment, the AUC values of saxagliptin and its active metabolite were 20% and 70% higher, respectively, than AUC values in subjects with normal renal function. Because increases of this magnitude are not considered to be clinically relevant, dosage adjustment in patients with mild renal impairment is not recommended. In subjects with moderate or severe renal impairment, the AUC values of saxagliptin and its active metabolite were up to 2.1- and 4.5-fold higher, respectively, than AUC values in subjects with normal renal function. To achieve plasma exposures of saxagliptin and its active metabolite similar to those in patients with normal renal function, the recommended dose is 2.5 mg once daily in patients with moderate and severe renal impairment, as well as in patients with end-stage renal disease requiring hemodialysis. Saxagliptin is removed by hemodialysis.
Hepatic Impairment
In subjects with hepatic impairment (Child-Pugh classes A, B, and C), mean Cmax and AUC of saxagliptin were up to 8% and 77% higher, respectively, compared to healthy matched controls following administration of a single 10 mg dose of saxagliptin. The corresponding Cmax and AUC of the active metabolite were up to 59% and 33% lower, respectively, compared to healthy matched controls. These differences are not considered to be clinically meaningful. No dosage adjustment is recommended for patients with hepatic impairment.
Body Mass Index
No dosage adjustment is recommended based on body mass index (BMI) which was not identified as a significant covariate on the apparent clearance of saxagliptin or its active metabolite in the population pharmacokinetic analysis.
Gender
No dosage adjustment is recommended based on gender. There were no differences observed in saxagliptin pharmacokinetics between males and females. Compared to males, females had approximately 25% higher exposure values for the active metabolite than males, but this difference is unlikely to be of clinical relevance. Gender was not identified as a significant covariate on the apparent clearance of saxagliptin and its active metabolite in the population pharmacokinetic analysis.
Geriatric
No dosage adjustment is recommended based on age alone. Elderly subjects (65-80 years) had 23% and 59% higher geometric mean Cmax and geometric mean AUC values, respectively, for saxagliptin than young subjects (18-40 years). Differences in active metabolite pharmacokinetics between elderly and young subjects generally reflected the differences observed in saxagliptin pharmacokinetics. The difference between the pharmacokinetics of saxagliptin and the active metabolite in young and elderly subjects is likely due to multiple factors including declining renal function and metabolic capacity with increasing age. Age was not identified as a significant covariate on the apparent clearance of saxagliptin and its active metabolite in the population pharmacokinetic analysis
Pediatric
Studies characterizing the pharmacokinetics of saxagliptin in pediatric patients have not been performed.
Race and Ethnicity
No dosage adjustment is recommended based on race. The population pharmacokinetic analysis compared the pharmacokinetics of saxagliptin and its active metabolite in 309 Caucasian subjects with 105 non-Caucasian subjects (consisting of six racial groups). No significant difference in the pharmacokinetics of saxagliptin and its active metabolite were detected between these two populations.
Drug-Drug Interactions
In Vitro Assessment of Drug Interactions
The metabolism of saxagliptin is primarily mediated by CYP3A4/5.
In in vitro studies, saxagliptin and its active metabolite did not inhibit CYP1A2, 2A6, 2B6, 2C9, 2C19, 2D6, 2E1, or 3A4, or induce CYP1A2, 2B6, 2C9, or 3A4. Therefore, saxagliptin is not expected to alter the metabolic clearance of coadministered drugs that are metabolized by these enzymes. Saxagliptin is a P-glycoprotein (P-gp) substrate but is not a significant inhibitor or inducer of P-gp.
The in vitro protein binding of saxagliptin and its active metabolite in human serum is negligible. Thus, protein binding would not have a meaningful influence on the pharmacokinetics of saxagliptin or other drugs.
In Vivo Assessment of Drug Interactions
Effects of Saxagliptin on Other Drugs
In studies conducted in healthy subjects, as described below, saxagliptin did not meaningfully alter the pharmacokinetics of metformin, glyburide, pioglitazone, digoxin, simvastatin, diltiazem, or ketoconazole.
Metformin: Coadministration of a single dose of saxagliptin (100 mg) and metformin (1000 mg), an hOCT-2 substrate, did not alter the pharmacokinetics of metformin in healthy subjects. Therefore, Onglyza is not an inhibitor of hOCT-2-mediated transport.
Glyburide: Coadministration of a single dose of saxagliptin (10 mg) and glyburide (5 mg), a CYP2C9 substrate, increased the plasma Cmax of glyburide by 16%; however, the AUC of glyburide was unchanged. Therefore, Onglyza does not meaningfully inhibit CYP2C9-mediated metabolism.
Pioglitazone: Coadministration of multiple once-daily doses of saxagliptin (10 mg) and pioglitazone (45 mg), a CYP2C8 substrate, increased the plasma Cmax of pioglitazone by 14%; however, the AUC of pioglitazone was unchanged.
Digoxin: Coadministration of multiple once-daily doses of saxagliptin (10 mg) and digoxin (0.25 mg), a P-gp substrate, did not alter the pharmacokinetics of digoxin. Therefore, Onglyza is not an inhibitor or inducer of P-gp-mediated transport.
Simvastatin: Coadministration of multiple once-daily doses of saxagliptin (10 mg) and simvastatin (40 mg), a CYP3A4/5 substrate, did not alter the pharmacokinetics of simvastatin. Therefore, Onglyza is not an inhibitor or inducer of CYP3A4/5-mediated metabolism.
Diltiazem: Coadministration of multiple once-daily doses of saxagliptin (10 mg) and diltiazem (360 mg long-acting formulation at steady state), a moderate inhibitor of CYP3A4/5, increased the plasma Cmax of diltiazem by 16%; however, the AUC of diltiazem was unchanged.
Ketoconazole: Coadministration of a single dose of saxagliptin (100 mg) and multiple doses of ketoconazole (200 mg every 12 hours at steady state), a strong inhibitor of CYP3A4/5 and P-gp, decreased the plasma Cmax and AUC of ketoconazole by 16% and 13%, respectively.
Effects of Other Drugs on Saxagliptin
Metformin: Coadministration of a single dose of saxagliptin (100 mg) and metformin (1000 mg), an hOCT-2 substrate, decreased the Cmax of saxagliptin by 21%; however, the AUC was unchanged.
Glyburide: Coadministration of a single dose of saxagliptin (10 mg) and glyburide (5 mg), a CYP2C9 substrate, increased the Cmax of saxagliptin by 8%; however, the AUC of saxagliptin was unchanged.
Pioglitazone: Coadministration of multiple once-daily doses of saxagliptin (10 mg) and pioglitazone (45 mg), a CYP2C8 (major) and CYP3A4 (minor) substrate, did not alter the pharmacokinetics of saxagliptin.
Digoxin: Coadministration of multiple once-daily doses of saxagliptin (10 mg) and digoxin (0.25 mg), a P-gp substrate, did not alter the pharmacokinetics of saxagliptin.
Simvastatin: Coadministration of multiple once-daily doses of saxagliptin (10 mg) and simvastatin (40 mg), a CYP3A4/5 substrate, increased the Cmax of saxagliptin by 21%; however, the AUC of saxagliptin was unchanged.
Diltiazem: Coadministration of a single dose of saxagliptin (10 mg) and diltiazem (360 mg long-acting formulation at steady state), a moderate inhibitor of CYP3A4/5, increased the Cmax of saxagliptin by 63% and the AUC by 2.1-fold. This was associated with a corresponding decrease in the Cmax and AUC of the active metabolite by 44% and 36%, respectively.
Ketoconazole: Coadministration of a single dose of saxagliptin (100 mg) and ketoconazole (200 mg every 12 hours at steady state), a strong inhibitor of CYP3A4/5 and P-gp, increased the Cmax for saxagliptin by 62% and the AUC by 2.5-fold. This was associated with a corresponding decrease in the Cmax and AUC of the active metabolite by 95% and 91%, respectively.
In another study, coadministration of a single dose of saxagliptin (20 mg) and ketoconazole (200 mg every 12 hours at steady state), increased the Cmax and AUC of saxagliptin by 2.4-fold and 3.7-fold, respectively. This was associated with a corresponding decrease in the Cmax and AUC of the active metabolite by 96% and 90%, respectively.
Rifampin: Coadministration of a single dose of saxagliptin (5 mg) and rifampin (600 mg QD at steady state) decreased the Cmax and AUC of saxagliptin by 53% and 76%, respectively, with a corresponding increase in Cmax (39%) but no significant change in the plasma AUC of the active metabolite.
Omeprazole: Coadministration of multiple once-daily doses of saxagliptin (10 mg) and omeprazole (40 mg), a CYP2C19 (major) and CYP3A4 substrate, an inhibitor of CYP2C19, and an inducer of MRP-3, did not alter the pharmacokinetics of saxagliptin.
Aluminum hydroxide + magnesium hydroxide + simethicone: Coadministration of a single dose of saxagliptin (10 mg) and a liquid containing aluminum hydroxide (2400 mg), magnesium hydroxide (2400 mg), and simethicone (240 mg) decreased the Cmax of saxagliptin by 26%; however, the AUC of saxagliptin was unchanged.
Famotidine: Administration of a single dose of saxagliptin (10 mg) 3 hours after a single dose of famotidine (40 mg), an inhibitor of hOCT-1, hOCT-2, and hOCT-3, increased the Cmax of saxagliptin by 14%; however, the AUC of saxagliptin was unchanged.
Nonclinical Toxicology
Carcinogenesis, Mutagenesis, Impairment of Fertility
Saxagliptin did not induce tumors in either mice (50, 250, and 600 mg/kg) or rats (25, 75, 150, and 300 mg/kg) at the highest doses evaluated. The highest doses evaluated in mice were equivalent to approximately 870 (males) and 1165 (females) times the human exposure at the MRHD of 5 mg/day. In rats, exposures were approximately 355 (males) and 2217 (females) times the MRHD.
Saxagliptin was not mutagenic or clastogenic with or without metabolic activation in an in vitro Ames bacterial assay, an in vitro cytogenetics assay in primary human lymphocytes, an in vivo oral micronucleus assay in rats, an in vivo oral DNA repair study in rats, and an oral in vivo/in vitro cytogenetics study in rat peripheral blood lymphocytes. The active metabolite was not mutagenic in an in vitro Ames bacterial assay.
In a rat fertility study, males were treated with oral gavage doses for 2 weeks prior to mating, during mating, and up to scheduled termination (approximately 4 weeks total) and females were treated with oral gavage doses for 2 weeks prior to mating through gestation day 7. No adverse effects on fertility were observed at exposures of approximately 603 (males) and 776 (females) times the MRHD. Higher doses that elicited maternal toxicity also increased fetal resorptions (approximately 2069 and 6138 times the MRHD). Additional effects on estrous cycling, fertility, ovulation, and implantation were observed at approximately 6138 times the MRHD.
Animal Toxicology
Saxagliptin produced adverse skin changes in the extremities of cynomolgus monkeys (scabs and/or ulceration of tail, digits, scrotum, and/or nose). Skin lesions were reversible at ≥20 times the MRHD but in some cases were irreversible and necrotizing at higher exposures. Adverse skin changes were not observed at exposures similar to (1 to 3 times) the MRHD of 5 mg. Clinical correlates to skin lesions in monkeys have not been observed in human clinical trials of saxagliptin.
Clinical Studies
Onglyza has been studied as monotherapy and in combination with metformin, glyburide, and thiazolidinedione (pioglitazone and rosiglitazone) therapy. Onglyza has not been studied in combination with insulin.
A total of 4148 patients with type 2 diabetes mellitus were randomized in six, double-blind, controlled clinical trials conducted to evaluate the safety and glycemic efficacy of Onglyza. A total of 3021 patients in these trials were treated with Onglyza. In these trials, the mean age was 54 years, and 71% of patients were Caucasian, 16% were Asian, 4% were black, and 9% were of other racial groups. An additional 423 patients, including 315 who received Onglyza, participated in a placebo-controlled, dose-ranging study of 6 to 12 weeks in duration.
In these six, double-blind trials, Onglyza was evaluated at doses of 2.5 mg and 5 mg once daily. Three of these trials also evaluated a saxagliptin dose of 10 mg daily. The 10 mg daily dose of saxagliptin did not provide greater efficacy than the 5 mg daily dose. Treatment with Onglyza at all doses produced clinically relevant and statistically significant improvements in hemoglobin A1c (A1C), fasting plasma glucose (FPG), and 2-hour postprandial glucose (PPG) following a standard oral glucose tolerance test (OGTT), compared to control. Reductions in A1C were seen across subgroups including gender, age, race, and baseline BMI.
Onglyza was not associated with significant changes from baseline in body weight or fasting serum lipids compared to placebo.
Monotherapy
A total of 766 patients with type 2 diabetes inadequately controlled on diet and exercise (A1C ≥7% to ≤10%) participated in two 24-week, double-blind, placebo-controlled trials evaluating the efficacy and safety of Onglyza monotherapy.
In the first trial, following a 2-week single-blind diet, exercise, and placebo lead-in period, 401 patients were randomized to 2.5 mg, 5 mg, or 10 mg of Onglyza or placebo. Patients who failed to meet specific glycemic goals during the study were treated with metformin rescue therapy, added on to placebo or Onglyza. Efficacy was evaluated at the last measurement prior to rescue therapy for patients needing rescue. Dose titration of Onglyza was not permitted.
Treatment with Onglyza 2.5 mg and 5 mg daily provided significant improvements in A1C, FPG, and PPG compared to placebo (Table 3). The percentage of patients who discontinued for lack of glycemic control or who were rescued for meeting prespecified glycemic criteria was 16% in the Onglyza 2.5 mg treatment group, 20% in the Onglyza 5 mg treatment group, and 26% in the placebo group.
Table 3: Glycemic Parameters at Week 24 in a Placebo-Controlled Study of Onglyza Monotherapy in Patients with Type 2 Diabetes*
| Efficacy Parameter | Onglyza 2.5 mg N=102 | Onglyza 5 mg N=106 | Placebo N=95 |
|---|---|---|---|
| * Intent-to-treat population using last observation on study or last observation prior to metformin rescue therapy for patients needing rescue. | |||
| †Least squares mean adjusted for baseline value. | |||
| c p-value <0.0001 compared to placebo | |||
| § p-value <0.05 compared to placebo | |||
| ¶ Significance was not tested for the 2-hour PPG for the 2.5 mg dose of Onglyza. | |||
| Hemoglobin A1C (%) | N=100 | N=103 | N=92 |
| Baseline (mean) | 7.9 | 8.0 | 7.9 |
| Change from baseline (adjusted mean†) | −0.4 | −0.5 | +0.2 |
| Difference from placebo (adjusted mean†) | −0.6c | −0.6c | |
| 95% Confidence Interval | (−0.9, −0.3) | (−0.9, −0.4) | |
| Percent of patients achieving A1C <7% | 35% (35/100) | 38% § (39/103) | 24% (22/92) |
| Fasting Plasma Glucose (mg/dL) | N=101 | N=105 | N=92 |
| Baseline (mean) | 178 | 171 | 172 |
| Change from baseline (adjusted mean†) | −15 | −9 | +6 |
| Difference from placebo (adjusted mean†) | −21 § | −15 § | |
| 95% Confidence Interval | (−31, −10) | (−25, −4) | |
| 2-hour Postprandial Glucose (mg/dL) | N=78 | N=84 | N=71 |
| Baseline (mean) | 279 | 278 | 283 |
| Change from baseline (adjusted mean†) | −45 | −43 | −6 |
| Difference from placebo (adjusted mean†) | −39 ¶ | −37 § | |
| 95% Confidence Interval | (−61, −16) | (−59, −15) | |
A second 24-week monotherapy trial was conducted to assess a range of dosing regimens for Onglyza. Treatment-naive patients with inadequately controlled diabetes (A1C ≥7% to ≤10%) underwent a 2-week, single-blind diet, exercise, and placebo lead-in period. A total of 365 patients were randomized to 2.5 mg every morning, 5 mg every morning, 2.5 mg with possible titration to 5 mg every morning, or 5 mg every evening of Onglyza, or placebo. Patients who failed to meet specific glycemic goals during the study were treated with metformin rescue therapy added on to placebo or Onglyza; the number of patients randomized per treatment group ranged from 71 to 74.
Treatment with either Onglyza 5 mg every morning or 5 mg every evening provided significant improvements in A1C versus placebo (mean placebo-corrected reductions of −0.4% and −0.3%, respectively). Treatment with Onglyza 2.5 mg every morning also provided significant improvement in A1C versus placebo (mean placebo-corrected reduction of −0.4%).
Combination Therapy
Add-On Combination Therapy with Metformin
A total of 743 patients with type 2 diabetes participated in this 24-week, randomized, double-blind, placebo-controlled trial to evaluate the efficacy and safety of Onglyza in combination with metformin in patients with inadequate glycemic control (A1C ≥7% and ≤10%) on metformin alone. To qualify for enrollment, patients were required to be on a stable dose of metformin (1500-2550 mg daily) for at least 8 weeks.
Patients who met eligibility criteria were enrolled in a single-blind, 2-week, dietary and exercise placebo lead-in period during which patients received metformin at their pre-study dose, up to 2500 mg daily, for the duration of the study. Following the lead-in period, eligible patients were randomized to 2.5 mg, 5 mg, or 10 mg of Onglyza or placebo in addition to their current dose of open-label metformin. Patients who failed to meet specific glycemic goals during the study were treated with pioglitazone rescue therapy, added on to existing study medications. Dose titrations of Onglyza and metformin were not permitted.
Onglyza 2.5 mg and 5 mg add-on to meformin provided significant improvements in A1C, FPG, and PPG compared with placebo add-on to metformin (Table 4). Mean changes from baseline for A1C over time and at endpoint are shown in Figure 1. The proportion of patients who discontinued for lack of glycemic control or who were rescued for meeting prespecified glycemic criteria was 15% in the Onglyza 2.5 mg add-on to metformin group, 13% in the Onglyza 5 mg add-on to metformin group, and 27% in the placebo add-on to metformin group.
Table 4: Glycemic Parameters at Week 24 in a Placebo-Controlled Study of Onglyza as Add-On Combination Therapy with Metformin*
| Efficacy Parameter | Onglyza 2.5 mg + Metformin N=192 | Onglyza 5 mg + Metformin N=191 | Placebo + Metformin N=179 |
|---|---|---|---|
| * Intent-to-treat population using last observation on study or last observation prior to pioglitazone rescue therapy for patients needing rescue. | |||
| †Least squares mean adjusted for baseline value. | |||
| c p-value <0.0001 compared to placebo + metformin | |||
| § p-value <0.05 compared to placebo + metformin | |||
| Hemoglobin A1C (%) | N=186 | N=186 | N=175 |
| Baseline (mean) | 8.1 | 8.1 | 8.1 |
| Change from baseline (adjusted mean†) | −0.6 | −0.7 | +0.1 |
| Difference from placebo (adjusted mean†) | −0.7c | −0.8c | |
| 95% Confidence Interval | (−0.9, −0.5) | (−1.0, −0.6) | |
| Percent of patients achieving A1C <7% | 37% § (69/186) | 44% § (81/186) | 17% (29/175) |
| Fasting Plasma Glucose (mg/dL) | N=188 | N=187 | N=176 |
| Baseline (mean) | 174 | 179 | 175 |
| Change from baseline (adjusted mean†) | −14 | −22 | +1 |
| Difference from placebo (adjusted mean†) | −16 § | −23 § | |
| 95% Confidence Interval | (−23, −9) | (−30, −16) | |
| 2-hour Postprandial Glucose (mg/dL) | N=155 | N=155 | N=135 |
| Baseline (mean) | 294 | 296 | 295 |
| Change from baseline (adjusted mean†) | −62 | −58 | −18 |
| Difference from placebo (adjusted mean†) | −44 § | −40 § | |
| 95% Confidence Interval | (−60, −27) | (−56, −24) | |
Figure 1: Mean Change from Baseline in A1C in a Placebo-Controlled Trial of Onglyza as Add-On Combination Therapy with Metformin*
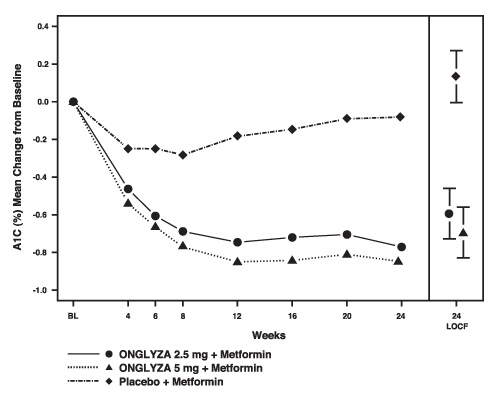
* Includes patients with a baseline and week 24 value.
Week 24 (LOCF) includes intent-to-treat population using last observation on study prior to pioglitazone rescue therapy for patients needing rescue. Mean change from baseline is adjusted for baseline value.
Add-On Combination Therapy with a Thiazolidinedione
A total of 565 patients with type 2 diabetes participated in this 24-week, randomized, double-blind, placebo-controlled trial to evaluate the efficacy and safety of Onglyza in combination with a thiazolidinedione (TZD) in patients with inadequate glycemic control (A1C ≥7% to ≤10.5%) on TZD alone. To qualify for enrollment, patients were required to be on a stable dose of pioglitazone (30-45 mg once daily) or rosiglitazone (4 mg once daily or 8 mg either once daily or in two divided doses of 4 mg) for at least 12 weeks.
Patients who met eligibility criteria were enrolled in a single-blind, 2-week, dietary and exercise placebo lead-in period during which patients received TZD at their pre-study dose for the duration of the study. Following the lead-in period, eligible patients were randomized to 2.5 mg or 5 mg of Onglyza or placebo in addition to their current dose of TZD. Patients who failed to meet specific glycemic goals during the study were treated with metformin rescue, added on to existing study medications. Dose titration of Onglyza or TZD was not permitted during the study. A change in TZD regimen from rosiglitazone to pioglitazone at specified, equivalent therapeutic doses was permitted at the investigator's discretion if believed to be medically appropriate.
Onglyza 2.5 mg and 5 mg add-on to TZD provided significant improvements in A1C, FPG, and PPG compared with placebo add-on to TZD (Table 5). The proportion of patients who discontinued for lack of glycemic control or who were rescued for meeting prespecified glycemic criteria was 10% in the Onglyza 2.5 mg add-on to TZD group, 6% for the Onglyza 5 mg add-on to TZD group, and 10% in the placebo add-on to TZD group.
Table 5: Glycemic Parameters at Week 24 in a Placebo-Controlled Study of Onglyza as Add-On Combination Therapy with a Thiazolidinedione*
| Efficacy Parameter | Onglyza 2.5 mg + TZD N=195 | Onglyza 5 mg + TZD N=186 | Placebo + TZD N=184 |
|---|---|---|---|
| * Intent-to-treat population using last observation on study or last observation prior to metformin rescue therapy for patients needing rescue. | |||
| †Least squares mean adjusted for baseline value. | |||
| c p-value <0.0001 compared to placebo + TZD | |||
| § p-value <0.05 compared to placebo + TZD | |||
| Hemoglobin A1C (%) | N=192 | N=183 | N=180 |
| Baseline (mean) | 8.3 | 8.4 | 8.2 |
| Change from baseline (adjusted mean†) | −0.7 | −0.9 | −0.3 |
| Difference from placebo (adjusted mean†) | −0.4 § | −0.6c | |
| 95% Confidence Interval | (−0.6, −0.2) | (−0.8, −0.4) | |
| Percent of patients achieving A1C <7% | 42% § (81/192) | 42% § (77/184) | 26% (46/180) |
| Fasting Plasma Glucose (mg/dL) | N=193 | N=185 | N=181 |
| Baseline (mean) | 163 | 160 | 162 |
| Change from baseline (adjusted mean†) | −14 | −17 | −3 |
| Difference from placebo (adjusted mean†) | −12 § | −15 § | |
| 95% Confidence Interval | (−20, −3) | (−23, −6) | |
| 2-hour Postprandial Glucose (mg/dL) | N=156 | N=134 | N=127 |
| Baseline (mean) | 296 | 303 | 291 |
| Change from baseline (adjusted mean†) | −55 | −65 | −15 |
| Difference from placebo (adjusted mean†) | −40 § | −50 § | |
| 95% Confidence Interval | (−56, −24) | (−66, −34) | |
Add-On Combination Therapy with Glyburide
A total of 768 patients with type 2 diabetes participated in this 24-week, randomized, double-blind, placebo-controlled trial to evaluate the efficacy and safety of Onglyza in combination with a sulfonylurea (SU) in patients with inadequate glycemic control at enrollment (A1C ≥7.5% to ≤10%) on a submaximal dose of SU alone. To qualify for enrollment, patients were required to be on a submaximal dose of SU for 2 months or greater. In this study, Onglyza in combination with a fixed, intermediate dose of SU was compared to titration to a higher dose of SU.
Patients who met eligibility criteria were enrolled in a single-blind, 4-week, dietary and exercise lead-in period, and placed on glyburide 7.5 mg once daily. Following the lead-in period, eligible patients with A1C ≥7% to ≤10% were randomized to either 2.5 mg or 5 mg of Onglyza add-on to 7.5 mg glyburide or to placebo plus a 10 mg total daily dose of glyburide. Patients who received placebo were eligible to have glyburide up-titrated to a total daily dose of 15 mg. Up-titration of glyburide was not permitted in patients who received Onglyza 2.5 mg or 5 mg. Glyburide could be down-titrated in any treatment group once during the 24-week study period due to hypoglycemia as deemed necessary by the investigator. Approximately 92% of patients in the placebo plus glyburide group were up-titrated to a final total daily dose of 15 mg during the first 4 weeks of the study period. Patients who failed to meet specific glycemic goals during the study were treated with metformin rescue, added on to existing study medication. Dose titration of Onglyza was not permitted during the study.
In combination with glyburide, Onglyza 2.5 mg and 5 mg provided significant improvements in A1C, FPG, and PPG compared with the placebo plus up-titrated glyburide group (Table 6). The proportion of patients who discontinued for lack of glycemic control or who were rescued for meeting prespecified glycemic criteria was 18% in the Onglyza 2.5 mg add-on to glyburide group, 17% in the Onglyza 5 mg add-on to glyburide group, and 30% in the placebo plus up-titrated glyburide group.
Table 6: Glycemic Parameters at Week 24 in a Placebo-Controlled Study of Onglyza as Add-On Combination Therapy with Glyburide*
| Efficacy Parameter | Onglyza 2.5 mg + Glyburide 7.5 mg N=248 | Onglyza 5 mg + Glyburide 7.5 mg N=253 | Placebo + Up-Titrated Glyburide N=267 |
|---|---|---|---|
| * Intent-to-treat population using last observation on study or last observation prior to metformin rescue therapy for patients needing rescue. | |||
| †Least squares mean adjusted for baseline value. | |||
| c p-value <0.0001 compared to placebo + up-titrated glyburide | |||
| § p-value <0.05 compared to placebo + up-titrated glyburide | |||
| Hemoglobin A1C (%) | N=246 | N=250 | N=264 |
| Baseline (mean) | 8.4 | 8.5 | 8.4 |
| Change from baseline (adjusted mean†) | −0.5 | −0.6 | +0.1 |
| Difference from up-titrated glyburide (adjusted mean†) | −0.6c | −0.7c | |
| 95% Confidence Interval | (−0.8, −0.5) | (−0.9, −0.6) | |
| Percent of patients achieving A1C <7% | 22% § (55/246) | 23% § (57/250) | 9% (24/264) |
| Fasting Plasma Glucose (mg/dL) | N=247 | N=252 | N=265 |
| Baseline (mean) | 170 | 175 | 174 |
| Change from baseline (adjusted mean†) | −7 | −10 | +1 |
| Difference from up-titrated glyburide (adjusted mean†) | −8 § | −10 § | |
| 95% Confidence Interval | (−14, −1) | (−17, −4) | |
| 2-hour Postprandial Glucose (mg/dL) | N=195 | N=202 | N=206 |
| Baseline (mean) | 309 | 315 | 323 |
| Change from baseline (adjusted mean†) | −31 | −34 | +8 |
| Difference from up-titrated glyburide (adjusted mean†) | −38 § | −42 § | |
| 95% Confidence Interval | (−50, −27) | (−53, −31) | |
Coadministration with Metformin in Treatment-Naive Patients
A total of 1306 treatment-naive patients with type 2 diabetes mellitus participated in this 24-week, randomized, double-blind, placebo-controlled trial to evaluate the efficacy and safety of Onglyza coadministered with metformin in patients with inadequate glycemic control (A1C ≥8% to ≤12%) on diet and exercise alone. Patients were required to be treatment-naive to be enrolled in this study.
Patients who met eligibility criteria were enrolled in a single-blind, 1-week, dietary and exercise placebo lead-in period. Patients were randomized to one of four treatment arms: Onglyza 5 mg + metformin 500 mg, saxagliptin 10 mg + metformin 500 mg, saxagliptin 10 mg + placebo, or metformin 500 mg + placebo. Onglyza was dosed once daily. In the 3 treatment groups using metformin, the metformin dose was up-titrated weekly in 500 mg per day increments, as tolerated, to a maximum of 2000 mg per day based on FPG. Patients who failed to meet specific glycemic goals during the studies were treated with pioglitazone rescue as add-on therapy.
Coadministration of Onglyza 5 mg plus metformin provided significant improvements in A1C, FPG, and PPG compared with placebo plus metformin (Table 7).
Table 7: Glycemic Parameters at Week 24 in a Placebo-Controlled Trial of Onglyza Coadministration with Metformin in Treatment-Naive Patients
| Efficacy Parameter | Onglyza 5 mg + Metformin N=320 | Placebo + Metformin N=328 |
|---|---|---|
| * Intent-to-treat population using last observation on study or last observation prior to pioglitazone rescue therapy for patients needing rescue. | ||
| †Least squares mean adjusted for baseline value. | ||
| c p-value <0.0001 compared to placebo + metformin | ||
| § p-value <0.05 compared to placebo + metformin | ||
| Hemoglobin A1C (%) | N=306 | N=313 |
| Baseline (mean) | 9.4 | 9.4 |
| Change from baseline (adjusted mean†) | −2.5 | −2.0 |
| Difference from placebo + metformin (adjusted mean†) | −0.5c | |
| 95% Confidence Interval | (−0.7, −0.4) | |
| Percent of patients achieving A1C <7% | 60% § (185/307) | 41% (129/314) |
| Fasting Plasma Glucose (mg/dL) | N=315 | N=320 |
| Baseline (mean) | 199 | 199 |
| Change from baseline (adjusted mean†) | −60 | −47 |
| Difference from placebo + metformin (adjusted mean†) | −13 § | |
| 95% Confidence Interval | (−19, −6) | |
| 2-hour Postprandial Glucose (mg/dL) | N=146 | N=141 |
| Baseline (mean) | 340 | 355 |
| Change from baseline (adjusted mean†) | −138 | −97 |
| Difference from placebo + metformin (adjusted mean†) | −41 § | |
| 95% Confidence Interval | (−57, −25) | |
How Supplied
Onglyza™ (saxagliptin) tablets have markings on both sides and are available in the strengths and packages listed in Table 8.
| Tablet Strength | Film-Coated Tablet Color/Shape | Tablet Markings | Package Size | NDC Code |
|---|---|---|---|---|
| 5 mg | pink biconvex, round | "5" on one side and "4215" on the reverse, in blue ink | Bottles of 30 Bottles of 90 Bottles of 500 Blister of 100 | 0003-4215-11 0003-4215-21 0003-4215-31 0003-4215-41 |
| 2.5 mg | pale yellow to light yellow biconvex, round | "2.5" on one side and "4214" on the reverse, in blue ink | Bottles of 30 Bottles of 90 | 0003-4214-11 0003-4214-21 |
Storage and Handling
Store at 20°-25°C (68°-77°F); excursions permitted to 15°-30°C (59°-86°F) [see USP Controlled Room Temperature].
Last Updated: 07/09
E.R. Squibb & Sons, L.L.C.
Detailed Info on Signs, Symptoms, Causes, Treatments of Diabetes
The information in this monograph is not intended to cover all possible uses, directions, precautions, drug interactions or adverse effects. This information is generalized and is not intended as specific medical advice. If you have questions about the medicines you are taking or would like more information, check with your doctor, pharmacist, or nurse.
back to: Browse all Medications for Diabetes
APA Reference
Staff, H.
(2009, July 31). Onglyza for Treatment of Diabetes - Full Prescribing Information, HealthyPlace. Retrieved
on 2026, March 7 from https://www.healthyplace.com/diabetes/medications/onglyza-saxagliptin-prescibing-information